Abstract

Background
Standard myeloablative conditioning treatment prior to allogeneic hematopoietic stem cell transplantation (alloHSCT) of children is associated with a considerable risk of severe adverse events (AEs). Previous clinical studies in adults confirmed that treosulfan-based conditioning has myeloablative, immunosuppressive and anti-neoplastic effects associated with favorable non-relapse mortality (NRM). Therefore, treosulfan-based conditioning treatment was prospectively evaluated in pediatric patients with hematological malignancies within an extended clinical phase II trial.
Patients andMethods
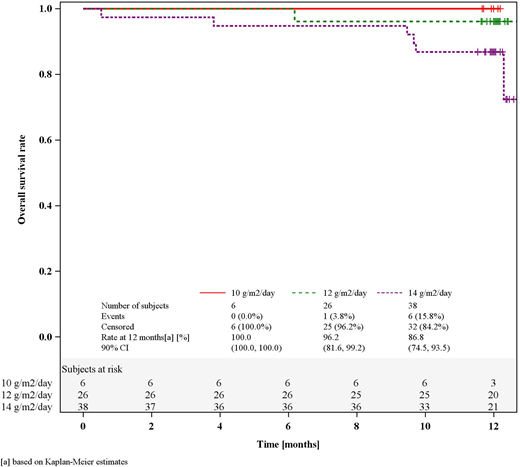
In this prospective, single-arm, open-label phase II trial we evaluated a treosulfan-based preparative regimen in pediatric patients with hematological malignancies undergoing alloHSCT. The trial was designed to assess safety and efficacy of a body surface area (BSA) adapted treosulfan dosing regimen of 10, 12 or 14 g/m2/day (according to individual BSA of ≤0.5, >0.5 to 1.0, or >1.0 m2) on Days -6 to -4. Objectives of the trial included overall survival (OS) based on Kaplan-Meier estimates, cumulative incidence (CI) of NRM and disease relapse/progression (RI). NRM was defined as the probability of dying after alloHSCT in the absence of persisting disease or previous occurrence of relapse/progression or graft failure. Moreover, the CI of acute/chronic graft versus host disease (a/cGvHD), the conditional CI of engraftment, Kaplan-Meier estimates of GvHD-free and Relapse/Progression-free Survival (GRFS) and cGvHD-free and Relapse/Progression-free Survival (CRFS), the incidence of complete donor type chimerism (defined as ≥ 95% donor cells), as well as frequencies of adverse events (AEs) until 100 days after alloHSCT were evaluated. Further, treosulfan concentration in plasma was analyzed to calculate AUC and Cmax in a subset of patients.
Results
Seventy pediatric patients with acute lymphoblastic leukemia (ALL [38.6%]), acute myeloid leukemia (AML, [41.4%]), myelodysplastic syndrome (MDS, [14.3%]), or juvenile myelomonocytic leukemia (JMML, [14.3%]) were enrolled between Nov-2014 and Apr-2016. The median patient age was 9.5 years (range 0-17 years) and median follow up was 12.0 months (range 11.5-17.7 months).
Patients received treosulfan intravenously at a dose of 10 g/m2/day (8.6%), 12 g/m2/day (37.1%), or 14 g/m2/day (54.3%). Treosulfan was combined with fludarabine only (7.1%) or fludarabine and thiotepa (92.9%) at the investigators' discretion.
The maximum conditional CI of granulocyte engraftment was 100.0% (90% CI: 97.7, 100.0). The incidence of complete donor-type chimerism at visit Day +28 was 94.2% (90% CI: 87.2, 98.0). OS at 12 months was 91.4% (90% CI: 83.9, 95.5). NRM at 12 months was only 1.4% (90% CI: 0.0, 3.8) and RI was 15.7% (90% CI: 8.6, 22.9). There was no statistical significant difference between the three dose groups with regard to any of these objectives.
Grade II to IV and III to IV aGvHD were 26.1% and 8.7%, respectively. At 12 months overall cGvHD was 24.8% and moderate/severe cGvHD was 18.8%. GRFS at 12 months was 64.7% (90% CI: 54.2, 73.4) and CRFS was 66.0% (90% CI: 55.5, 74.6).
The three most common CTCAE terms of at least grade III were mucositis oral (41.4%), infections and infestations - other (28.6%), and nausea (17.1%). One (1.4%) patient developed hepatic sinusoidal occlusion syndrome (grade II acc. to Jones) and recovered after 22 days. Frequencies of AEs with at least CTCAE grade III apparently correlated with increasing dose group. However, median AUC was comparable between the three different dose groups (1287 mg*hr/L [10g/ m2], 1268 mg*hr/L [12g/m2] and 1461mg*hr/L [14g/m2]) as evaluated in a subset of 58 patients. Median Cmax was also comparable between the different dose groups (628µg/mL [10g/m2], 583µg/mL [12g/m2] and 656µg/mL [14g/m2]).
Conclusions
The 12-month follow-up data of this phase II trial confirm that treosulfan-based conditioning with BSA-adapted dosing was safe and effective in pediatric patients with hematological malignancies. The cumulative incidence of OS and NRM compared favorably to those reported for other conditioning regimens. Treosulfan/fludarabin/thiotepa is therefore considered to be a reasonable alternative for myeloablative conditioning in this pediatric patient population.
(Funded by medac GmbH, MC-FludT.17/M, EudraCT no: 2013-003604-39; ClinicalTrials.gov identifier: NCT02333058).
Kalwak:medac: Other: travel grants; Sanofi: Other: travel grants. Bader:Riemser: Research Funding; Medac: Patents & Royalties, Research Funding; Neovii: Research Funding; Cellgene: Consultancy; Novartis: Consultancy, Speakers Bureau. Gruhn:Jazz Pharmaceuticals: Honoraria. Patrick:medac: Other: Funding for EBMT conference fees and accomodation. Sykora:Aventis-Behring: Research Funding; medac: Research Funding. Corbacioglu:Gentium: Consultancy, Honoraria; Jazz Pharmaceuticals: Consultancy, Honoraria. Locatelli:Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; bluebird bio: Consultancy; Bellicum: Consultancy, Membership on an entity's Board of Directors or advisory committees; Miltenyi: Honoraria; Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees. Kremens:DSMC for industry driven clinical study: Consultancy; Miltenyi Biotec Germany: Consultancy. Vora:Pfizer: Other: Advisory board; Medac: Other: Advisory board; Novartis: Other: Advisory board; Amgen: Other: Advisory board; Jazz: Other: Advisory board.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal